Optimizing PCM Medicare Billing for Clinic Revenue Growth
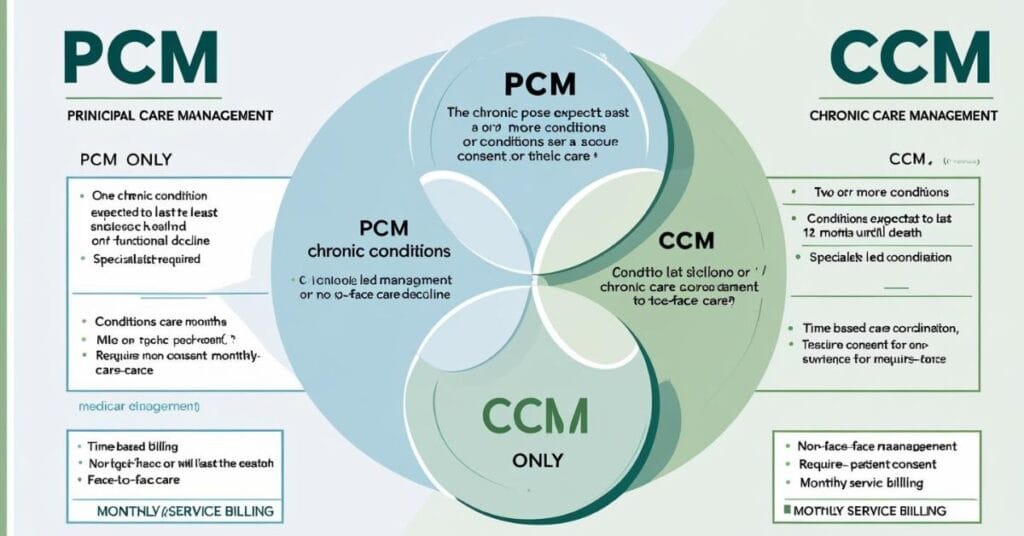
Principal Care Management (PCM) is actually a solid opportunity for clinics looking to enhance revenue while delivering structured, condition-specific support to Medicare patients. Unlike Chronic Care Management (CCM), PCM lets providers bill for care coordination tied to a single complex chronic condition.
With proper billing, EMR-integrated workflows, and documentation, PCM services can turn into a reliable monthly revenue stream. CMS continues to emphasize value-based reimbursement strategies, so accurate PCM billing is really important for practices. Physicians managing patients with just one qualifying chronic condition can, in fact, streamline time-based care tasks using CPT codes 99424–99427. This guide breaks down key operational practices, CMS billing compliance, EMR alignment, and how SmartCare360 supports physician workflows under Medicare PCM rules.
Medicare Eligibility Requirements for PCM Enrollment
To qualify:
- Medicare patient must have one serious chronic condition
- The condition should last at least 3 months
- It should place the patient at significant risk of hospitalization or death
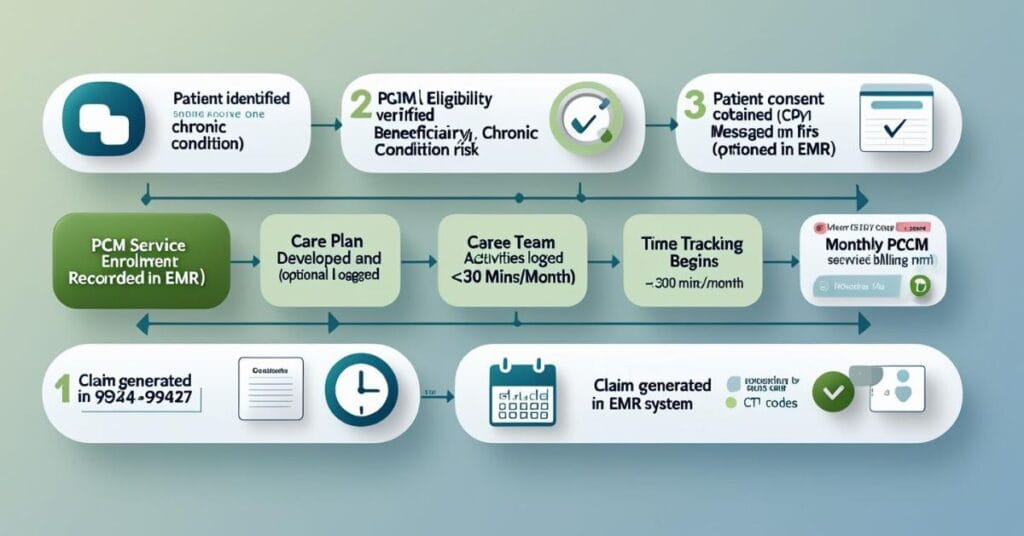
- Patient consent (verbal or written) is required
Common examples include advanced COPD, heart failure, or diabetic complications managed by one specialty.
CMS Focus on Single Complex Chronic Conditions
CMS introduced PCM to support patients whose conditions fall outside dual-chronic CCM eligibility. It creates, in fact, a billing path for specialist-driven care when CCM doesn’t apply.
- PCM and CCM can’t be billed at the same time for the same patient.
- How to Bill PCM Services Correctly Under Medicare
- CMS Billing Guidelines for PCM Claims Submission
Use the following CPT codes:
- 99424: 30 minutes of physician or QHP time (first 30 minutes per month)
- 99425: Each extra 30 minutes
- 99426–99427: For clinical staff time under supervision
- Only bill once per calendar month. Time has to be tracked in the EMR and meet the minimum for each code.
EMR Workflow Integration for PCM Time Tracking
- Tracks non-face-to-face time as it happens
- Notifies when 30-minute minimum is reached
- Flags duplicate billing risks (like with CCM or RPM)
Avoiding Denials and Coding Overlaps With CCM or RPM
- PCM and CCM are billed in the same month
- Time thresholds (like 30 mins for 99424) aren’t met
- There’s no record of actual clinical activities
- Set up EMR alerts for concurrent care codes
- Only assign PCM to patients with one qualifying condition
- Keep PCM and RPM tasks clearly separated
2025 Medicare PCM Reimbursement Rates and Profitability
- 99424: ~$80/month
- 99425: ~$60 (per added 30 mins)
- 99426–99427: ~$60–$40 (for staff time)
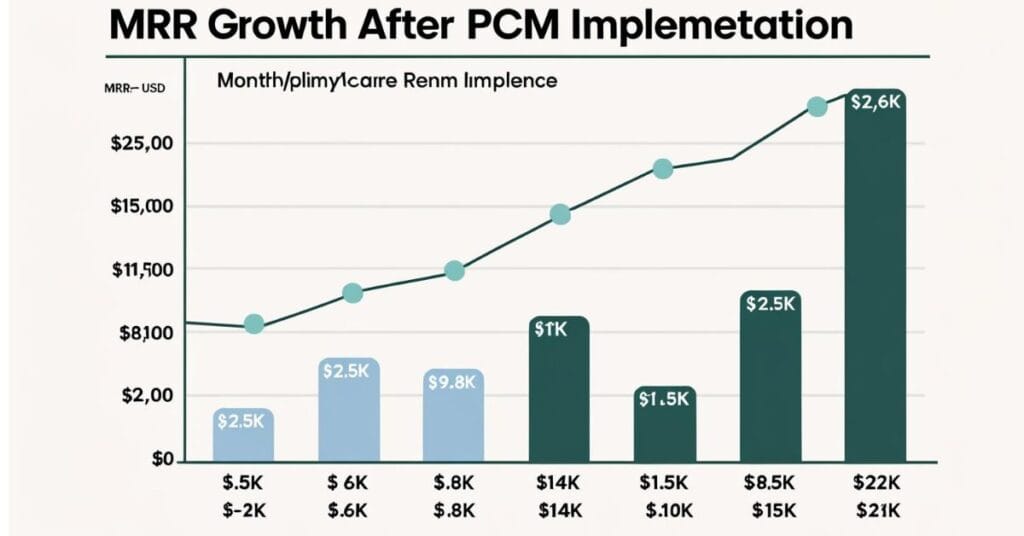
Net Revenue per PCM Patient: Clinic-Level Scenario
- Monthly PCM revenue = $80 x 60 = $4,800
- Staff time: 30–60 minutes per patient, tracked in EMR
- Annual PCM income = $57,600 (from 60 PCM patients)
Scaling PCM Across Specialties to Boost MRR
- Pulmonology (COPD)
- Neurology (Parkinson’s, epilepsy)
- Cardiology (CHF)
- Endocrinology (diabetes with complications)
PCM Documentation Guidelines Medicare Requires
- Documentation for PCM has to include:
- Time logs with start and end times
- What clinical actions were taken
- Patient consent and initial care plan
- Physician or specialist involvement
Avoiding Common Documentation Errors in Audits
Common mistakes include:
- Not logging time properly
- No record of interventions
- Too vague care plan language
- Billing overlaps between PCM, CCM, and RPM
Templates for PCM Note Compliance in EMRs
Use structured fields like:
Drop-downs for condition-specific goals
Auto-filled timestamps for PCM tasks
Prebuilt care summaries
These templates, in fact, help notes pass CMS review without slowing down your charting.
Integrating PCM Into Multispecialty Care Workflows
Roles of Primary and Specialist Physicians in PCM
- A specialist managing the dominant condition
- A primary care doctor with focused responsibility
- Use EMRs to define roles and avoid claim conflicts.
- Referral Coordination and Care Plan Updates
- PCM requires close coordination:
- Specialists must update PCPs on changes
- Shared EMR notes or summary reports help handoffs
SmartCare360’s Role in Streamlining PCM Operations
- Tracking PCM eligibility and renewals
- Capturing time and documentation within EMRs
- Billing alerts to prevent overlaps
- Monthly claims prep and audit support
FAQ's
How much clinical staff time is required to bill for PCM services?
To bill for the initial PCM service (CPT code 99424), a minimum of 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional is required per calendar month. Additional time can be billed using add-on codes.
Can a physician bill for an E/M service and PCM on the same day?
Yes, a physician can bill for an Evaluation and Management (E/M) service and PCM services on the same day, provided the E/M service is distinct and separately identifiable from the PCM services. Modifier 25 should be appended to the E/M code to indicate a significant, separately identifiable evaluation and management service by the same physician on the same day of a procedure or other service.
What are the key documentation elements required by Medicare for PCM?
Key documentation elements include evidence of patient consent, a comprehensive care plan, detailed records of clinical staff time spent (at least 30 minutes per month), specific interventions performed, and records of communication with the patient or caregiver.
What are common reasons for PCM claim denials?
Common reasons for PCM claim denials include insufficient documentation of time spent, lack of clear evidence of patient consent, incorrect CPT or ICD-10 coding, failure to demonstrate medical necessity for PCM, or absence of a developed and managed care plan.












